Evidence, and Evidence-Based Practices and Findings
Jim Grizzell,
MBA, MA, MCHES, ACSM-EP, FACHA
jimgrizzell@healthedpartners.org
Contents
Introduction........................................................................................................................................ 1
Importance
of Using “Evidence-Based Practice and Findings for CHES® and MCHES®.................................... 1
Types
of Evidence................................................................................................................................ 2
Anecdotal:
Not “Evidence-Informed” or “Evidence-Based”.................................................................. 2
Evidence-Informed......................................................................................................................... 3
Evidence-Based............................................................................................................................. 4
Steps
to Finding Evidence...................................................................................................................... 6
Reasons
Evidence-Based May Not be Used............................................................................................. 9
Summary............................................................................................................................................ 9
Thought
/ Critical Thinking Questions..................................................................................................... 9
Glossary
of Terms................................................................................................................................ 9
References
and Resources.................................................................................................................... 9
Introduction
The
Physical Activity Guidelines for
Americans has moved from evidence-informed in 2008 to evidence-based
in the 2nd edition published in November 20181. An emphasis in the continuing education
self-study course, The “Evidence-Based”
Physical Activity Guidelines for Americans (2nd edition) (2018)2, is to show how evidence
was gathered, the findings and resulting guidelines for 1) physical activity
and 2) health education/promotion to increase regular physical activity. This
paper gives an overview of evidence used for interventions to avoid harm and
improve health.
Importance of Using
Evidence-Based Practices and Findings for CHES®, MCHES® and CPH
Evidence-based is
emphasized because Certified Health Education Specialists (CHES®), the Master
Certified Health Education Specialists (MCHES®) Certified in Public Health (CPH)
and are expected to use evidence-based
practices. “Evidence” and “evidence-based” are stated In three of the seven
areas of responsibility of the Health Education
Specialist Practice Analysis (HESPA) 2015 Competencies3 for CHES® and
the MCHES®. And there are four sub-competencies (see
bullet point items below, two competencies are “Advance-1, for MCHES®) stating that CHES® and
the MCHES® should identify, apply and use evidence-based
findings. “Evidence” and “evidence-based” are stated six time in four of the 10
domain areas of the CPH Content Outline.4 NOTE: the term evidence-informed is not listed in the HESPA
Responsibilities and Competencies or CPH Content Outline.
Health Education Specialist Practice Analysis
(HESPA) 2015 Competencies
Area II: Plan Health Education/Promotion
·
2.3.3 Apply
principles of evidence-based practice
in selecting and/or designing strategies/interventions (Advance-1).
Area V: Administer and Manage Health
Education/Promotion
·
5.4.2 Identify evidence to justify programs
Area VII: Communicate, Promote, and Advocate
for Health, Health Education/Promotion and the Profession
·
7.3.5 Use evidence-based
findings in policy analysis
·
7.3.6
Develop policies to promote health using evidence-based
findings (Advance-1)
The
Responsibilities and Competencies for Health Education Specialists (web
page) have Areas of
Responsibility, Competencies and Sub-competencies for Health Education
Specialists 2015 (pdf,
note color coding for Advanced-1
and Advanced-2).
Certified
in Public Health Content Outline
Domain
Area: Evidence-based Approaches to Public Health
14. Apply evidence-based
theories, concepts, and models from a range of social and behavioral
disciplines in the development and evaluation of health programs, policies and
interventions
Domain
Area: Public Health Biology and Human Disease Risk
1. Apply evidence-based
biological concepts to inform public health laws, policies, and regulations
Domain
Area: Program Planning and Evaluation
10. Apply evidence-based
practices to program planning, implementation and evaluation
13. Plan evidence-based
interventions to meet established program goals and objectives
19. Use available evidence
to inform effective teamwork and team-based practices
Domain
Area: Policy in Public Health
5. Use scientific evidence,
best practices, stakeholder input, or public opinion data to inform policy and
program decision-making
Additionally, in 2001 Rimer, Glanz and
Rasband5 described why using evidence-based practices is important. They
wrote “Health educators and behavioral scientists should care about
evidence-based practice. Our goal is to improve the health of the public. Given
a shortage of resources, we must invest wisely in interventions that are most
likely to work. Moreover, we do not want to harm people by knowingly exposing
them to interventions that do not work, especially when there are proven
effective strategies. Using interventions that evidence shows are ineffective
not only wastes the resources invested in them but also crowds out alternative
actions. The best interventions are those with the greatest chance of changing
something that will make a desired difference.”
Types of Evidence
Anecdotal: Not “Evidence-Informed” or “Evidence-Based”
For
comparisons, it may be useful to see descriptions of health promotion practice
and findings that are not objective research evidence. Below are examples of how not evidence-based/informed might be described.
Key text to consider noting are in bold
and underlined.
From Richard Troiano, PhD (2008 PA
Guidelines Advisory Committee member) GWU Grand Rounds presentation in 2008.6
“. . .
public health practice . . , is moving towards a science-based, evidence-based
paradigm so that we don’t just kind
of do what we think is good, but we really have a strong evidentiary
base to support it.”
From US DHHS Office of Assistant
Secretary for Planning and Evaluation7
“In the
absence of evidence-based interventions, and often even when evidence-based
approaches exist, program operators frequently rely primarily on their personal experiences and good intentions
without careful consideration of related research evidence. While past
experience is valuable, ignoring existing evidence and developmental theory can
lead to missed opportunities, unintended results, and inefficient progress.”
From International Union for Health
Promotion and Education8
“The report concludes that programmes . . . are largely driven by “informed guesswork, expert hunches,
. . .”11
From
the journal Health Promotion Practice9
“Evidence-based practice is an
extension of evidence- based medicine, which moves
from “uninformed intuition, unsystematic clinical experience, and pathophysiologic rationale”
as the basis of clinical decision making, emphasizing instead the assessment of
clinical research evidence.”
From article in journal Health
Education and Behavior5
“Do we make decisions based on what
does or does not “work” according to the evidence or based on tradition,
intuition, precedent, and available resources? Would we replace what we feel
works best with what we know is better, based on evidence?”
Evidence-Informed
Below are examples of how evidence-informed has
been described. Key text to consider noting are in bold and underlined.
From Richard Troiano, PhD (2008 PA
Guidelines Advisory Committee member) GWU Grand Rounds presentation in 2008.6
“The other thing, if we just
look at those studies, those 560 studies on adiposity, you can see that
there’s quite a variety of study designs incorporated in that number. This
again reflects on why we had to
evolve to this evidence-informed concept
from an evidence-based concept. So out of the 560 studies, a little less than 200 were experimental
but that is both randomized and non-randomized studies.

So, if you took the drug trial
model and said I’m only going to rely upon randomized control trials, when
you’re looking at behaviors, you really don’t have much that you can go with.
So, you really need to cast a wider net and realize the tradeoffs when you’re
looking at observational and cross-sectional studies, but they do have
information to contribute.”

From National Alzheimer’s and Dementia
Resource Center (NADRC)10, 12
For consideration as evidence-informed,
an intervention must have
·
substantial research evidence that demonstrates
an ability to improve, maintain, or slow the decline in the health and
functional status of older people or family caregivers.
Evidence-informed interventions
(1)
have been tested by at least one quasi-experimental
design with a comparison group, with at least 50 participants; OR
(2)
have been adapted from evidence-based
interventions.
From article in journal British
Journal of Social Work11
“Evidence-informed practice (EIP) should be understood as excluding non-scientific prejudices and
superstitions, but also as leaving ample room for clinical experience
as well as the constructive and imaginative judgements of practitioners and
clients who are in constant interaction and dialogue with one another. . . . practitioners
will become knowledgeable of a wide range of sources—empirical studies, case
studies and clinical insights—and use them in creative ways throughout the
intervention process.”
Evidence-Based
Below are examples of how evidence-based has
been described. Key text to consider noting are in bold and underlined.
From article in journal Health
Education & Behavior5
. . . make decisions based on what does . . . “work” according to the evidence . .
. replace what we feel works best
with what we know is better, based on evidence?
“Jenicek called evidence-based public health “the process of systematically finding, appraising, and using
contemporaneous research findings as the basis for decisions in public health.”
From National Alzheimer’s and Dementia
Resource Center (NADRC) and Administration on Community Living (ACL) to receive
grants10, 12
For consideration as evidence-based, an
intervention must have
·
been tested
through randomized controlled trials and
(1)
be effective at improving, maintaining, or slowing the decline in
the health or functional status of older people or family caregivers;
(2)
be suitable for deployment through community-based human services
organizations and involve nonclinical workers or volunteers in the delivery of
the intervention;
(3)
have results published in a peer-reviewed scientific journal; and
(4) be translated
into practice and ready for distribution through community-based human services
organizations.
ACL Definition of
Evidence-Based Programs
·
Demonstrated through evaluation to be
effective for improving the health and well-being or reducing disease,
disability and/or injury among older adults; and
·
Proven effective with older adult population,
using Experimental or Quasi-Experimental Design;* and
·
Research results published in a peer-review
journal; and
·
Fully translated** in one or more community
site(s); and
·
Includes developed dissemination products that
are available to the public.
*Experimental
designs use random assignment and a control group. Quasi-experimental designs
do not use random assignment.
**For
purposes of the Title III-D definitions, being “fully translated in one or more
community sites” means that the evidence-based program in question has been
carried out at the community level (with fidelity to the published research) at
least once before. Sites should only consider programs that have been shown to
be effective within a real-world community setting.
Note: ACL
distinguishes between “evidence-based program” and “evidence-based
service/practice.” Services and practices are within programs. See answer to
question 8 of the Frequently Asked Questions on this page https://acl.gov/programs/health-wellness/disease-prevention. The “Resources”
section on this page also gives three items for “Understanding and Finding Evidence-Based
Programs.”
From Physical Activity Guidelines for Americans (2nd
edition)13
Use “. . . a
methodology informed by best practices for systematic reviews (SRs) developed
by the United States Department of Agriculture’s (USDA) Nutrition Evidence Library
(NEL),1 the Agency for Healthcare Research and Quality (AHRQ),2
the Cochrane Collaboration,3 and the Health and Medicine Division of
the National Academies of Sciences, Engineering, and Medicine SR standards to review, evaluate, and synthesize published,
peer-reviewed physical activity research. The literature review team’s
rigorous, protocol-driven methodology was designed to maximize transparency,
minimize bias, and ensure the SRs conducted by the Committee were relevant,
timely, and of high quality. Using this evidence-based
approach enabled compliance with the Data Quality Act,5 which states
that federal agencies must ensure the quality, objectivity, utility, and
integrity of the information used to form federal guidance.”6
Steps to Finding Evidence
The techniques of evidence-based medicine
involve these steps:14
(a)
asking research questions to precisely defining
the patient or population problem and the information required to solve it,
(b)
conducting an efficient literature search,
(c)
selecting high-quality relevant studies,
(d)
applying rules of evidence to determine their
validity,
(e)
describing the content of the study along with
its strengths and weaknesses, and
(f)
extracting the health message for application
to the problem.
The Physical Activity Guidelines for
American Advisory Committee followed each of the steps listed below. It was
instructed to examine the scientific literature. The Executive
Summary15 states that the Committee conducted detailed
searches of the scientific literature, evaluated and discussed at length the
quality of the evidence, and developed conclusions based on the evidence as a
whole. The Committee used state-of-the-art methods for systematic reviews to
address 38 research questions and 104 subquestions. Part E.
Systematic Review Literature Search Methodology16 details
the process used are described approaches to reviewing research. Part E lists
and describes the process as:
Step 1: Develop systematic Review Questions
Step 2: Develop Systematic Review Strategy
Step 3: Search, Screen, and Select Evidence to Review
Step 4: Abstract Data and Assess Quality and Risk of Bias
Step 5: Describe the Evidence
Step 6: Complete Evidence Portfolios and Draft Scientific Report
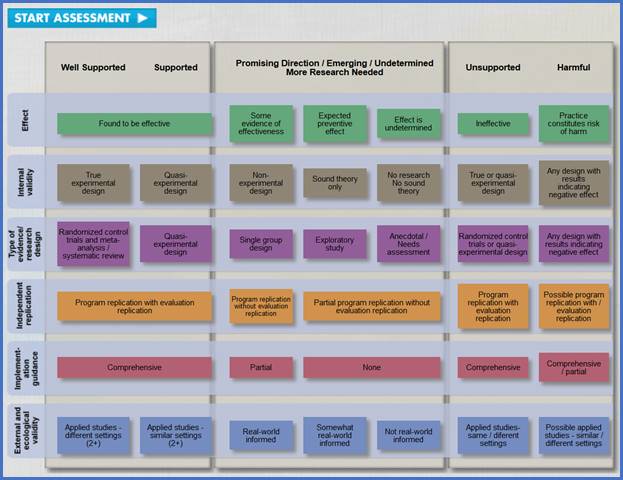
A set of steps to assess evidence is in CDC’s online tool, Continuum of Evidence of Effectiveness.16 The Continuum of Evidence of Effectiveness clarifies and defines standards of the Best Available Research Evidence. In Understanding Evidence, the Continuum is applied specifically to the field of violence prevention, but it can be used to inform evidence-based decision-making in a wide range of health-related areas. Evidence is assessed from harmful and unsupported through well supported. The dimensions covered include:
· Effect (effectiveness) – effective through practice constitutes risk of harm
· Internal validity – true experimental design through no research and research with results of negative effect
· Types of evidence/research (randomized control and meta-analysis / systematic review) through anecdotal / Needs assessment and design with negative effect
· Independent replication – program replication with evaluation through possible replication / evaluation
· Implementation guidance – comprehensive through none or partial
· External and ecological validity – two or more studies with different settings through not real world and possible same or different settings
Questions in the assessment include:
1.
Are there any indications from research or
practice that this strategy has been associated with harmful effects?
2.
Does the available research on this strategy
include two or more well-conducted studies (Randomized Control Trials or
Quasi-experimental designs)?
3.
Have any of these studies shown significant
effects in areas that you are concerned about?
4.
Is the study you are reviewing a Randomized
Control Trial?
5.
Does the study you are reviewing use a
Quasi-Experimental design?
6.
Has the program or strategy been implemented
in more than one setting?
7.
Has the program or strategy been evaluated in almost exactly the same
way in both of these settings?
8.
Are any of the following formal systems in
place to support implementation of the program or strategy?
9.
If formal systems to support implementation
are in place, are these resources available and accessible?
10.
Has the program or strategy been implemented
in two or more applied ("real world") settings?
11.
Does the strategy include components that are
consistent with an applied setting (i.e. uses materials and resources that
would be available/appropriate in an applied setting)?
12.
Has the strategy been implemented in ways that
mirror conditions of the “real world” (in other words, delivered in ways that
it would have to be delivered in real world settings)?
Click on the image of the ASSESSMENT tool on the next page to go to the web page with the assessment. The Iink is https://vetoviolence.cdc.gov/apps/evidence/continuumIntro.aspx#&panel1-8.
NOTE: the tool may work best with the Microsoft Edge browser. The tool uses Adobe Flash Player which may need to be installed on your computer if you find the highlighted boxes don’t appear after completing the assessment.
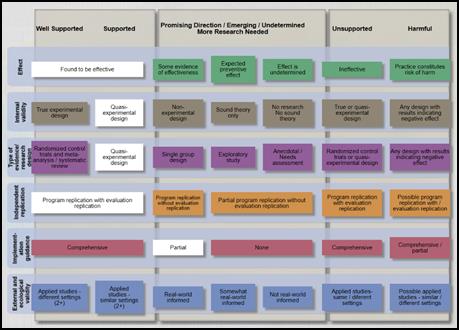
You can click through and answer the questions without having to login, use as a Guest. Once you complete the assessment several colored (green, brown, purple, etc.) should be white showing you where your answers mapped to each dimension. This will give you an indicator of the strength of evidence informing the various aspects of the strategy you are considering. Click on the white boxes to learn more about your results.
Reasons Evidence-Based May Not be Used
From
keynote presentation: “Evidence-Based Public Health” for 2018 Nevada Public
Health Association conference.17
·
Formal training - <50% of public health
workers
·
No single credential or license required – but
voluntary credentialing as Certified in Public Health, Certified Health
Education Specialist, Master Certified Health Education Specialist
·
Evidence-based practice needs multidisciplinary
approach and needs multiple perspectives
·
Interventions are based on: 1) political and
media pressure, 2) anecdotal evidence, 3) “the way it’s always been done
·
Barriers are: 1) lack of funds, skilled
personnel, incentives, time; 2) limited buy-in from leadership and elected
officials
From Pathways to
“Evidence-Informed” Policy and Practice: A Framework for Action7
“ . . . hindered by a lack of good-quality, synthesized evidence,
capacity to apply the evidence, and organizational support and resources to
make evidence-based decisions.”
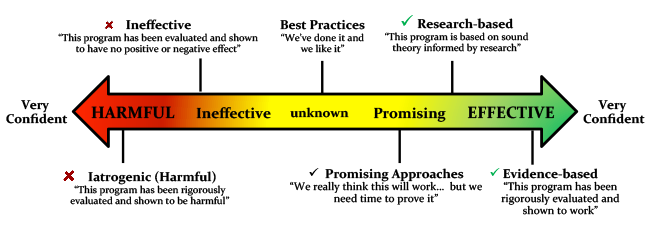
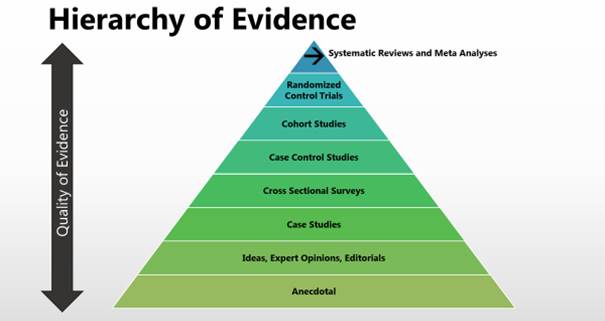
A Visual Description of Evidence: the Hierarchy
of Evidence18
The
hierarchy of evidence reflects the relative authority of the literature. Relative
authority can be depicted in a pyramid format where the base of the pyramid
includes research with the lowest quality of evidence (anecdotal) and the top
of the pyramid with the highest quality of evidence ( systematic review, meta-analyses
and random control trials). Quality of evidence refers to the range of bias and
opportunity for research to have systematic errors. For example, anecdotal or
opinions and editorials can have a significant level of bias based on the
author and their experience. On the other hand, randomized controlled trials or
systematic reviews control for bias through prescribed study designs and
represent the highest level of evidence.
Summary
Rimer, Glanz and Rasband4, and the
National Commission for Health Education Credentialing3 state that it is
important for health educators and health promotion professionals to use
evidence-based practices. There is a range of evidence to use for selecting
and/or designing strategies/interventions and policies. Likely least effective and
could harm and waste resources are interventions based on personal experiences,
tradition, intuition, doing what is thought to be good, and lack of resources.
Evidence-informed findings can provide support for interventions that could
improve, maintain or slow decline in health. Application of evidence-informed findings
may leave room for experience, and constructive and imaginative judgements. Interventions
and policies from the process of asking research questions, using a systematic
literature review strategy, assessing quality of data, describing the evidence
and applying the evidence is the basis of evidence-based practices.
Thought / Critical Thinking Questions
Think of a group, committee, organization or health
education/promotion team you might or do work with. Describe the group purpose,
members’ knowledge and experience, and your role (e.g., leader, topic expert,
member).
For the group, team organization you
described in the previous question and considering your role, how would you explain
anecdotal, evidence-informed and evidence-based? How do you or might you influence
the members t use evidence-based practices and
findings for interventions, strategies, programs and policies.? Explain how do
you or would you influence the members to use evidence-based practices and
findings for strategies, programs and policies?
Glossary of Terms*
Anecdotal - evidence in the form of stories that
people tell about what has happened to them.
Case-control study - A type
of epidemiologic study design in which participants are selected based on the
presence or absence of a specific outcome of interest, such as cancer or
diabetes. The participant's past physical activity practices are assessed, and
the association between past physical activity and presence of the outcome is
determined.
Cross-sectional study - A type
of epidemiologic study that compares and evaluates specific groups or
populations at a single point in time.
Intervention - Any
kind of planned activity or group of activities (including programs, policies,
and laws) designed to prevent disease or injury or promote health in a group of
people, about which a single summary conclusion can be drawn.
Observational study - A study
in which outcomes are measured but no attempt is made to change the outcome.
The two most commonly used designs for observational studies are case-control
studies and prospective cohort studies.
Prospective cohort study - A type
of epidemiologic study in which the practices of the enrolled subjects are determined,
and the subjects are followed (or observed) for the development of selected
outcomes. It differs from randomized controlled trials in that the exposure is
not assigned by the researchers.
Retrospective study - A study
in which the outcomes have occurred before the study data collection has begun.
Fidelity - Fidelity is the degree to which a program, practice, or
policy is conducted in the way that it was intended to be conducted. This is
particularly important during replication, where fidelity is the extent to
which a program, practice, or policy being conducted in a new setting mirrors
the way it was conducted in its original setting.
Meta-analysis - A review of a focused question that follows rigorous
methodological criteria and uses statistical techniques to combine data from
studies on that question.
Quasi-experimental - Experiments based on sound theory, and typically have comparison
groups (but no random assignment of participants to condition), and/or
multiple measurement points (e.g., pre-post measures, longitudinal design).
Random
Control Trial (RCT) –
From Physical Activity Guidelines for Americans: A type of
study design in which participants are randomly grouped on the basis of an
investigator-assigned exposure of interest, such as physical activity. For
example, among a group of eligible participants, investigators may randomly
assign them to exercise at three levels: no activity, moderate-intensity
activity, and vigorous-intensity activity. The participants are then followed
over time to assess the outcome of interest, such as change in abdominal fat.
From
Understanding Evidence: A trial in which participants are assigned to
control or experimental (receive strategy) groups at random, meaning that all
members of the sample must have an equal chance of being selected
for either the control or experimental groups (i.e..
Flipping a coin, where “heads” means participants are assigned to the control
group and “tails” means they are assigned to the experimental group). This way,
it can be assumed that the two groups are equivalent and there are no
systematic differences between them, which increases the likelihood that any
differences in outcomes are due to the program, practice, or policy and not
some other variable(s) that the groups differ on.
Systematic
Review -
From Physical Activity Guidelines for Americans: A review of a clearly defined question that uses systematic and
explicit methods to identify, select, and critically evaluate relevant
research, and to collect and analyze data from the studies includedin
the review.
From CDC’s
Understanding Evidence: The assembly, critical appraisal, and
synthesis of all relevant studies of a specific program, practice, or policy in
order to assess its overall effectiveness, feasibility, and “best practices” in
its implementation.
* Most definitions are from the Physical Activity
Guidelines for Americans (2nd edition) are available in the Scientific Report, Appendix H-1. Glossary of
Term [PDF – 874 KB] https://health.gov/paguidelines/second-edition/report/pdf/19_H_Appendix_1_Glossary_of_Terms.pdf.
CDC’s Understanding Evidence definitions
in its “Resources” web page https://vetoviolence.cdc.gov/apps/evidence/resourcesIntro.aspx#&panel1-7. Scroll down to the box “GLOSSARY.”
References and Resources
1. Office of Disease Prevention and Health
Promotion (2018). Physical activity guidelines for Americans (2nd
edition). https://health.gov/paguidelines/. Accessed on April 15, 2019.
2. Health Education Partners (2019). The evidence-based physical activity guidelines for Americans. www.healthedpartners.org/ceu/ebpag . Accessed on April 20, 2019.
3. National Commission for Health Education
Credentialing, Inc. (2015). Responsibilities and competencies for health education,
https://www.nchec.org/responsibilities-and-competencies. Areas
of Responsibility, Competencies and Sub-competencies for Health Education
Specialists 2015. Accessed on April 15, 2019.
4 National Board of Public Health Examiners
(2019). CPH content outline. https://www.nbphe.org/cph-content-outline. Accessed on May 8, 2019.
5 4. Rimer, B, DrPHKaren
Glanz. K, PhD, MPHGloria Rasband, G, BA, MA, (2001). Searching
for evidence about health education and
health behavior interventions.
Health Education
& Behavior: pp. 231-248. , First
Published Apr 1, 2001. https://journals.sagepub.com/doi/pdf/10.1177/109019810102800208
Accessed on April 18,
2015.
6 5. Troiano,
R. PhD. PA Guidelines (1st edition), Advisory Committee member
(2008). The 2008 physical activity guidelines
for Americans: development and dissemination of new federal evidence-informed recommendation.
George Washington University, December 9, 2008 GWU Grand Rounds
presentation
Original and Current links for the mp3 audio
and transcript
![]()
www.kaisernetwork.org/health_cast/hcast_index.cfm?display=detail&hc=3084
kaisernetwork.org/health_cast/uploaded_files/120908_gwu_troiana_transcript.pdf
- www.kaisernetwork.org no longer available –
Audio: www.healthedpartners.org/ceu/pag2nd/ei-eb/pag01_02_troiano_audio.mp3
Original Transcript: www.healthedpartners.org/ceu/pag2nd/ei-eb/pag01_02_troiano_transcript.pdf
PowerPoint: www.healthedpartners.org/ceu/pag2nd/ei-eb/pag01_02_troiano_powerpoint.pdf
Transcript with the audio’s times of
corresponding slides: www.healthedpartners.org/ceu/pag2nd/ei-eb/pag01_02_troiano_transcript_with
slide times.pdf
7. U.S.
Department of Health and Human Services, Office of the Assistant Secretary for
Planning and Evaluation, Office of Human Services Policy (2013). Best intentions
are not enough: techniques for using research and data to develop prevention programs.
https://aspe.hhs.gov/system/files/pdf/139251/rb_bestintention.pdf. Accessed
on April 16, 2019.
8. Bowen S, Zwi AB (2005)
Pathways to “evidence-informed” policy and practice: a framework for action.
PLoS Med 2(7): e166. https://doi.org/10.1371/journal.pmed.0020166. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1140676/ Accessed on April 19, 2019.
9. Hill, E.K., MLS, AHIP, Alpi, K.M. MLS, MPH AHIP, Auerbach,
Marilyn, AMLS MPH, DrPH. (2010). Evidence-based practice
in health education and promotion: a review and introduction to resources,
Health Promotion Practice. May 2010 Vol. 11, No. 3, 358-366 DOI:
10.1177/1524839908328993 © 2010 Society for Public Health Education
10.
Administration on Aging. National Alzheimer’s and Dementia Resource Center. 2018 NADRC: grantee-implemented evidence-based
and evidence-informediInterventions. https://nadrc.acl.gov/sites/default/files/uploads/docs/EBEIIntervention2018final508revReadOnly.docx. https://nadrc.acl.gov/node/140. Access on April 16, 2019.
11. Nevo,
I., Slonim-Nevo, Vered. The myth of evidence-based practice: towards evidence-informed
practice. The
British Journal of Social Work, Volume 41, Issue 6, September 2011,
Pages 1176–1197, https://doi.org/10.1093/bjsw/bcq149.
Published: 24 January 2011. https://academic.oup.com/bjsw/article/41/6/1176/1720835.
Accessed on April 16, 2019.
12. Administration on Aging. Health promotion. https://acl.gov/programs/health-wellness/disease-prevention#future. Accessed on April 17, 2019
13. Office
of Disease Prevention and Health Promotion. Physical Activity Guidelines for
Americans (2nd edition (2018), Scientific report, part e. systematic
review literature search methodology. https://health.gov/paguidelines/second-edition/report/pdf/06_E_Systematic_Review_Literature_Search_Methodology.pdf. Accessed
on April 15, 2019.
14. Olson, E. A. (1996).
Evidence-based practice: a new approach to teaching the integration of research
and practice in gerontology. Educational Gerontology, 22, 523-537.
15. Office
of Disease Prevention and Health Promotion. Physical Activity Guidelines for
Americans (2nd edition), Scientific report, part a. executive summary
(2015). https://health.gov/paguidelines/second-edition/report/pdf/02_A_Executive_Summary.pdf. Accessed on April 15, 2019.
16. Center
for Disease Control and Prevention. Injury Prevention & and Control:
Division of Violence Prevention. Understanding evidence: continuum of evidence
of effectiveness. https://vetoviolence.cdc.gov/apps/evidence/continuumIntro.aspx#&panel1-8. Accessed
on April 23, 2019.
17.
Grizzell, J. (2018). Nevada public health association, keynote presentation:
evidence-based public health. www.healthedpartners.org/cocreators/npha. Accessed
on April 17, 2019.
18.
National Library of Medicine. (2019). From problem to presentation:
evidence-based public health. https://nnlm.gov/classes/problem-prevention-evidence-based-public-health. Accessed
on May 2, 2019.
Additional
Resources
Toolkit on Evidence-Based Programming for Seniors (Community
Research Center for Senior Health)
A comprehensive guide on finding and implementing evidence-based
programs in a community setting.
http://www.evidencetoprograms.com/
National
Council on Aging Evidence-Based Program Resources
Guides to understanding, implementing, and building a business
case for evidence-based programs.
https://www.ncoa.org/center-for-healthy-aging/basics-of-evidence-based-programs/
Evidence-Based Leadership Council
This organization represents a small but notable group of
evidence-based programs that are shown to improve older adult health.
Evidence-Based Programs 101 (one-page
pdf)
http://www.eblcprograms.org/docs/pdfs/EBPs_101.pdf
The Evidence Continuum
https://www.nationalservice.gov/resources/evaluation/evidence-continuum
https://youtu.be/fzF08edFXmc
Experimental Design: Evidence-based Programs
http://www.episcenter.psu.edu/research/experimentaldesign
The Differences Between CHES® and CPH
https://www.nchec.org/cph-vs-ches